How to Fix Your Jaw Pain – 2023 Deep Dive Into TMJ Pain
Jaw pain/TMJ pain – what is it and how do we treat it?
Temporomandibular joint dysfunction, commonly known as TMD, refers to a group of disorders affecting the temporomandibular joint, which connects the jawbone to the skull. TMJ dysfunction can lead to various symptoms, with jaw pain being one of the most prevalent. Individuals with TMJ issues may experience discomfort or tenderness in the jaw joint, difficulty in opening or closing the mouth, clicking or popping sounds during jaw movement, and even headaches or earaches. This condition can significantly impact one’s quality of life, interfering with everyday activities like eating and speaking. While the exact causes of TMJ dysfunction can vary, factors such as jaw misalignment, teeth grinding, arthritis, and jaw injuries are commonly associated with this condition. Understanding TMJ and its potential causes is vital for proper diagnosis and effective management of this often-painful condition
TMJ Overview
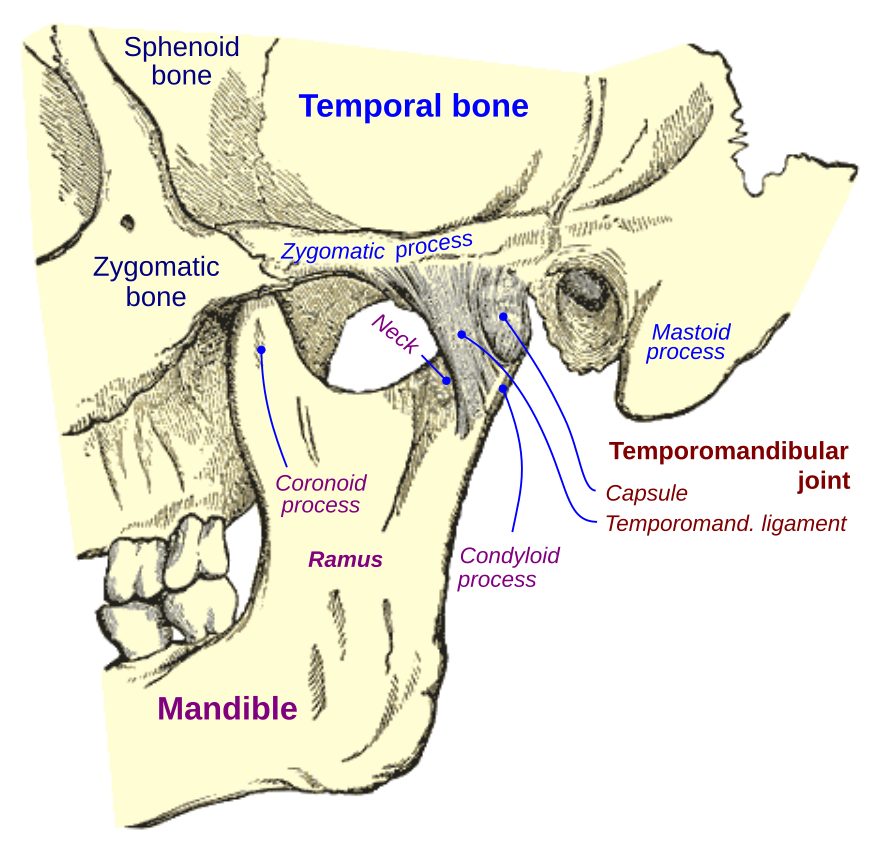
The temporomandibular joint (TMJ) is a complex joint located on each side of the head, just in front of the ears. It is responsible for the movement of the jaw, enabling essential functions such as chewing, speaking, and swallowing. The TMJ consists of several components, including the mandible (lower jaw bone), temporal bone (skull bone), articular disc, muscles, and ligaments.
The muscles surrounding the TMJ play a crucial role in its function and stability. The muscles responsible for jaw movement are divided into two groups: the muscles of mastication and the muscles of facial expression. The muscles of mastication, such as the temporalis, masseter, and medial pterygoid muscles, are primarily responsible for the actual movement of the jaw during chewing. The muscles of facial expression, including the orbicularis oris and buccinator muscles, assist in controlling facial movements.
Ligaments are strong bands of fibrous tissue that connect bones and provide stability to joints. In the TMJ, two main ligaments are involved: the temporomandibular ligament and the lateral ligament. The temporomandibular ligament runs from the zygomatic arch (cheekbone) to the mandible, helping to prevent excessive backward movement of the jaw. The lateral ligament is located on the outside of the joint and provides additional stability.
Located between the mandible and the temporal bone, the articular disc is a fibrous structure that acts as a cushion and helps to distribute forces within the joint. This disc is composed of dense connective tissue and has a complex shape that allows smooth movement of the jaw. Dysfunction or irritation of the TMJ can occur when any of these components are affected.
TMJ dysfunction can be caused by a variety of factors. Misalignment of the jaw joint, which can occur due to developmental issues or trauma, can lead to abnormal movement and place stress on the joint structures. Excessive grinding or clenching of the teeth, known as bruxism, can strain the TMJ and associated muscles, leading to dysfunction. Additionally, trauma to the jaw, such as a direct blow or dislocation, can damage the ligaments, muscles, or the articular disc, causing pain and dysfunction.
The Temporomandibular Joint
The TMJ allows for various movements that are essential for functions like chewing, speaking, and swallowing. The primary movements of the TMJ include:
- Hinge Movement (Opening and Closing): The TMJ acts as a hinge joint, enabling the mouth to open and close. This movement is primarily controlled by the action of the muscles of mastication, such as the temporalis and masseter muscles. The hinge movement allows for basic functions like biting, chewing, and speaking.
- Gliding Movement (Protrusion and Retraction): In addition to hinge-like movements, the TMJ also allows for gliding or sliding motions. This movement is responsible for the forward protrusion of the mandible (lower jaw) and its retraction back to its resting position. The lateral pterygoid muscles play a significant role in the gliding movement of the TMJ.
- Lateral Movement (Side-to-Side): The TMJ permits lateral or sideways movements of the mandible. This movement allows for grinding or shifting the teeth from side to side during chewing. It is controlled by coordinated actions of the lateral pterygoid muscles on each side.
These movements of the TMJ are coordinated and precise, involving the interaction of muscles, ligaments, and the articular disc. They are essential for proper functioning of the jaw, ensuring efficient chewing, speaking, and swallowing. Any dysfunction or imbalance in the TMJ can result in pain, clicking or popping sounds, limited movement, or discomfort during these activities
TMJ Anatomy
- Temporalis muscle:
- Origin: Temporal fossa and temporal lines of the parietal and frontal bones.
- Insertion: Coronoid process and anterior border of the ramus of the mandible.
- Function: The temporalis muscle is responsible for elevating the mandible (closing the mouth) and retracting the mandible (moving it backward).
- Masseter muscle:
- Origin: Zygomatic arch and maxilla.
- Insertion: Angle and lateral surface of the ramus of the mandible.
- Function: The masseter muscle is the primary muscle involved in the elevation of the mandible (closing the mouth) and contributes to the process of chewing.
- Medial pterygoid muscle:
- Origin: Medial surface of the lateral pterygoid plate, palatine bone, and maxilla.
- Insertion: Medial surface of the angle of the mandible.
- Function: The medial pterygoid muscle assists in the elevation of the mandible (closing the mouth) and contributes to lateral jaw movements during chewing.
- Lateral pterygoid muscle:
- Origin: Superior head: Greater wing of sphenoid bone. Inferior head: Lateral surface of the lateral pterygoid plate.
- Insertion: Superior head: Articular disc of the TMJ. Inferior head: Neck of the mandible.
- Function: The lateral pterygoid muscle plays a crucial role in jaw movements. The superior head assists in the depression and protrusion of the mandible, while the inferior head aids in the lateral deviation of the mandible and assists with opening the mouth.
- Digastric muscle:
- Origin: Anterior belly: Digastric fossa of the mandible. Posterior belly: Mastoid notch of the temporal bone.
- Insertion: Intermediate tendon connected to the hyoid bone.
- Function: The digastric muscle helps with the depression of the mandible (opening the mouth) and stabilizes the hyoid bone during swallowing and speaking.
- Mylohyoid muscle:
- Origin: Mylohyoid line of the mandible.
- Insertion: Hyoid bone and median raphe.
- Function: The mylohyoid muscle assists in the elevation of the floor of the mouth, elevation of the hyoid bone during swallowing, and plays a role in jaw stabilization.
Understanding the insertion, origin, and function of these muscles provides insights into their involvement in the movements and stability of the TMJ. Dysfunction or imbalance in these muscles can contribute to TMJ-related issues, highlighting the importance of proper evaluation and management when dealing with TMJ pain or dysfunction
Causes Of TMJ Pain
Temporomandibular joint (TMJ) pain can manifest as discomfort, tenderness, or aching sensations in the jaw joint and surrounding areas. It can significantly impact daily activities such as chewing, speaking, and even yawning. The causes of TMJ pain can vary widely, ranging from mechanical factors like jaw misalignment and teeth grinding to underlying conditions such as arthritis or jaw injuries. Understanding the potential causes is crucial for accurate diagnosis and effective treatment. Below, we provide a comprehensive list of common factors that can contribute to TMJ pain.
- Trauma or Injury: Direct impact or trauma to the jaw joint area, such as a blow or accident, can lead to TMJ dysfunction. This can cause misalignment of the joint, damage to the disc, or other structural abnormalities.
- Bruxism (Teeth Grinding or Clenching): Persistent teeth grinding or clenching, often done unconsciously during sleep or due to stress, can put excessive pressure on the TMJ and its surrounding structures, leading to dysfunction. Bruxism can also contribute to the displacement or damage of the TMJ disc.
- Arthritis: Various forms of arthritis, such as osteoarthritis or rheumatoid arthritis, can affect the TMJ. Arthritic conditions can cause inflammation, joint degeneration, and damage to the cartilage within the joint, including the TMJ disc.
- Degenerative Joint Disease: Over time, the TMJ can experience wear and tear, leading to degenerative changes. This can include the degeneration of the TMJ disc, which may result in functional impairment and TMJ dysfunction.
- Disc Displacement: The TMJ disc, which acts as a cushion between the condyle of the mandible and the temporal bone, can become displaced or dislocated. This can occur due to trauma, excessive stress on the joint, or structural abnormalities. Disc displacement can lead to pain, clicking or popping sounds, and restricted jaw movement.
- Muscle Imbalances or Tension: Imbalances or excessive tension in the muscles surrounding the TMJ, such as the temporalis, masseter, or lateral pterygoid muscles, can contribute to TMJ dysfunction. Muscle-related causes may involve abnormal muscle activity, spasms, or trigger points that affect the proper functioning of the TMJ and its disc.
TMJ dysfunction can have various causes, and taking a holistic approach to its treatment is crucial. It’s important to recognize that the health of the temporomandibular joint (TMJ) is influenced by multiple factors, not just the joint itself. One significant factor is stress, which can lead to jaw clenching and teeth grinding (bruxism). A stressed individual may unknowingly engage in these habits, placing excessive pressure on the TMJ and contributing to dysfunction. Therefore, addressing TMJ issues requires considering the broader context of a person’s overall well-being, including stress management techniques, relaxation exercises, and lifestyle modifications. Incorporating a holistic approach takes into account not only the joint’s condition but also the surrounding muscles, alignment, posture, and emotional factors that impact the TMJ.
TMJ Conservative Treatment/Rehab
When performing TMJ exercises, it is important to focus on proper technique and listen to your body. It is normal to feel some mild soreness or discomfort during and after the exercises, but you should never experience sharp pain. If you do feel pain, it is important to stop the exercise and consult with a healthcare professional.
The goal of TMJ exercises is to gradually increase the number of repetitions and sets over time. Starting with a lower number of repetitions and sets is perfectly fine, as it allows your jaw muscles to adapt and avoids overexertion. As you progress, aim to gradually increase the number of repetitions or sets rather than pushing for maximum effort in a single session.
Remember, consistency is key when it comes to TMJ exercises. It is recommended to perform the exercises on a regular basis, ideally daily or as advised by your healthcare professional. Consistent practice will help to improve jaw mobility, strengthen the muscles, and promote better function of the temporomandibular joint.
Always pay attention to your body’s response and adjust the intensity of the exercises accordingly. If you experience increased soreness or discomfort that persists or worsens over time, it is important to consult with a healthcare professional for further guidance and evaluation.
Overall, the progression of TMJ exercises should be gradual and focused on increasing the number of repetitions and sets over time, while avoiding pain and allowing for proper muscle recovery. Patience and consistency will yield better results in managing TMJ dysfunction.
Sample Exercises and Stretches
- Jaw Opening and Closing:
- Place the tip of your tongue on the roof of your mouth behind your front teeth.
- Gently open your mouth as wide as you comfortably can, without causing pain.
- Hold the open position for a few seconds, then slowly close your mouth.
- Repeat this exercise 5-10 times.
- Jaw Side-to-Side Movement:
- Keep your teeth slightly apart and gently shift your jaw to the right, maintaining a relaxed position.
- Hold the position for a few seconds, then shift your jaw to the left.
- Repeat this exercise 5-10 times on each side.
- Jaw Protrusion and Retraction:
- Keep your teeth slightly apart and gently move your jaw forward, as if you are trying to touch your bottom teeth with your top teeth.
- Hold the protruded position for a few seconds, then slowly retract your jaw back to the resting position.
- Repeat this exercise 5-10 times.
- Resistive Jaw Opening:
- Place your thumb under your chin.
- Gently press upward with your thumb while trying to open your mouth against the resistance.
- Hold the resistance for a few seconds, then relax.
- Repeat this exercise 5-10 times.
All numbers here are an example, and not a set in stone number. Listen to your body and how it is responding to the exercises. If it is easy, go for more, if it is too difficult, decrease the amount.
- Jaw Stretch:
- Place the tip of your tongue on the roof of your mouth just behind your front teeth.
- Gently open your mouth as wide as you comfortably can, creating a stretch in the jaw muscles.
- Hold the stretch for 5-10 seconds, then slowly close your mouth.
- Repeat the stretch 5-10 times.
- Chin to Chest Stretch:
- Sit or stand with good posture.
- Slowly lower your chin towards your chest until you feel a stretch in the back of your neck and jaw.
- Hold the stretch for 10-15 seconds, then slowly lift your head back to the starting position.
- Repeat the stretch 5-10 times.
- Jaw Side Stretch:
- Place one hand on the side of your jaw near your ear.
- Gently apply pressure to the jaw, pushing it to the side.
- Slowly tilt your head in the opposite direction, away from the hand that is providing pressure.
- Hold the stretch for 10-15 seconds, then release.
- Repeat the stretch on the other side, using the opposite hand.
- Tongue Press:
- Place the tip of your tongue on the roof of your mouth just behind your front teeth.
- Press your tongue against the roof of your mouth with a firm but comfortable pressure.
- Hold the tongue press for 5-10 seconds, then release.
- Repeat the press 5-10 times.
Remember to perform these stretches with control and without causing pain. If you experience increased pain or discomfort during or after the stretches, it is advisable to consult with a healthcare professional or a physical therapist who specializes in TMJ disorders. They can provide further guidance and recommend appropriate stretches based on your individual needs and condition.
TMJ Treatment
When it comes to treating TMJ dysfunction, it is important to understand that there is no one-size-fits-all approach. Each individual’s condition may vary, and the treatment plan should be tailored to their specific needs. Typically, healthcare professionals follow a conservative care approach before considering more invasive options. The goal is to start with the least invasive and most conservative treatments and progress to more invasive measures only if necessary. Conservative treatments may include self-care measures, lifestyle modifications, medications, and the use of oral splints or mouthguards. If symptoms persist or worsen, additional interventions such as physical therapy, dental procedures, stress management techniques, medication injections, or, as a last resort, surgery may be considered. The progression from conservative care to more invasive treatments ensures that individuals receive the most appropriate and effective treatment while minimizing potential risks and complications. It is essential to work closely with healthcare professionals specializing in TMJ dysfunction to determine the best course of action based on individual circumstances.
- Self-Care and Lifestyle Modifications: In mild cases, self-care measures can be effective in relieving TMJ symptoms. These may include avoiding hard or chewy foods, practicing relaxation techniques to reduce stress and tension, applying moist heat or cold packs to the jaw area, and maintaining good posture.
- Medications: Over-the-counter pain relievers such as nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation associated with TMJ dysfunction. Muscle relaxants may be prescribed to alleviate muscle spasms or tension.
- Oral Splints or Mouthguards: Dentists often recommend the use of oral splints or mouthguards to treat TMJ dysfunction. These devices help to stabilize the jaw joint, reduce grinding or clenching of the teeth, and relieve pressure on the TMJ.
- Physical Therapy: Physical therapy can be beneficial for TMJ dysfunction, especially when muscular imbalances or tightness contribute to the condition. Therapeutic exercises, stretching techniques, and manual therapy may be employed to improve jaw mobility, strengthen the muscles, and alleviate pain.
- Dental Procedures: In some cases, dental treatments may be necessary to correct misalignments or bite issues that contribute to TMJ dysfunction. Orthodontic treatments, dental crowns, or other dental procedures may be recommended to restore proper alignment and function of the jaw.
- Stress Management: Since stress and tension can exacerbate TMJ symptoms, stress management techniques such as relaxation exercises, meditation, counseling, or behavioral therapy may be helpful in managing TMJ dysfunction.
- Medication Injections: In certain cases, corticosteroid injections directly into the TMJ may be used to reduce inflammation and provide pain relief. This approach is typically reserved for severe or persistent cases of TMJ dysfunction.
- Surgery: Surgical intervention for TMJ dysfunction is considered a last resort when conservative treatments have not been successful. Surgery may be performed to repair or remove damaged joint structures, reposition the jaw, or address structural abnormalities.
For more on treatment, here is an article.
Conclusion
TMJ pain is a common condition that can significantly impact one’s quality of life. The temporomandibular joint, along with its associated structures such as muscles, ligaments, and discs, plays a vital role in proper jaw function. TMJ pain can arise from a variety of causes, including trauma, bruxism, arthritis, disc displacement, and muscle imbalances. Understanding the complexity of TMJ pain and the factors contributing to its development is crucial in formulating an effective treatment plan. It is essential to approach TMJ pain holistically, considering not only the joint itself but also the surrounding muscles, alignment, posture, and emotional well-being. Treatment options range from self-care measures and lifestyle modifications to medications, oral splints, physical therapy, dental procedures, and, in severe cases, surgical interventions. Each individual may require a personalized approach to address their specific needs. By working closely with healthcare professionals specializing in TMJ disorders, individuals can find relief from pain, restore proper jaw function, and improve their overall well-being. Remember, early intervention and seeking professional guidance are key to managing TMJ pain effectively and promoting a healthier, pain-free life.






